| What is MACRA? |
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) is a law that transformed the Medicare payment system for physicians. MACRA shifts Medicare to a value based system, tying your Medicare payments to cost and quality performance by replacing the flawed Sustainable Growth Rate (SGR) physician fee update formula.
| Why MACRA? |
The goal is to improve care for Medicare patients by transitioning the payment system from volume to value beginning in 2019.
| What is the Quality Payment Program? |
The Quality Payment Program policy through CMS will reform Medicare Part B payments for more than 600,000 clinicians across the country, and is a major step in improving care across the entire health care delivery system. Based on their practice size, specialty, location, or patient population, clinicians can decide how they want to participate in the Quality Payment Program. There are two models to choose from:
Merit-based Incentive Payment System (MIPS)
- If you decide to participate in traditional Medicare, you may earn a performance-based payment adjustment through MIPS.
- This streamlines existing Medicare quality programs including Physician Quality Reporting Program (PQRS), the Value-Based Payment Modifier (VM), and the Medicare EHR Incentive Program (MU) into one program. Most clinicians will fall under MIPS during the first year.
Advanced Alternative Payment Models (APMs)
- If you decide to take part in an Advanced APM, you may earn a Medicare incentive payment for participating in an innovative payment model.
- This provides different pathways for physicians to participate that incentivizes quality and value.
| Who Participates in MIPS and Who is Excluded? |
| Who Participates | Who is Excluded |
| Medicare Part B clinicians billing more than $30,000 a year and providing care for more than 100 Medicare patients a year. These clinicians include Physicians, Physician Assistants, Nurse Practitioners, Clinical Nurse Specialists, and Certified Registered Nurse Anesthetists. |
|
| What are the Requirements? |
| Reduced Requirements for Improvement Activities Performance Category |
|
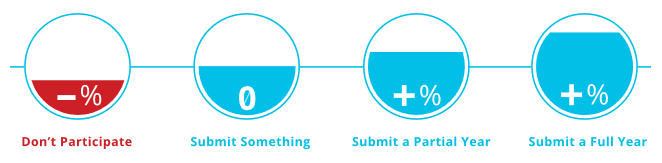
| Partial Participation |
|
| Full Participation |
|
| Top 9 Things to Do to Position Your Practice to Succeed under MACRA |
- Learn about MACRA and the new Quality Payment Program
- Attest to Medicare EHR Incentive Program, a.k.a. Meaningful Use (MU) of your EHR
- Implement a formal process to improve Physician Quality Reporting System (PQRS) and MU quality measures
- Review your Quality Resource Use Report (QRUR)
- Use a CMS-certified vendor to collect Consumer Assessment of Healthcare Providers & Systems (CAHPS) survey data
- Understand Patient-Centered Medical Home (PCMH), a care delivery model, and begin implementing in your practice
- Participate in a medical neighborhood and provide care coordination
- Risk stratify your patients and implement care management for high risk patients
- Reach out to EqualizeRCM Services (ERCM) to learn more about other recommendations and implement them in your practice
References
- Bogart, D. (2018). MACRA and MIPS. Austin: EqualizeRCM Services.
- American College of Physicians (ACP). (n.d.). MACRA Explained. Retrieved from American College of Physicians: https://www.acponline.org/practice-resources/business-resources/payment/medicare/macra.
- Centers for Medicare & Medicaid Services (CMS.gov). (2018, May 30). MACRA. Retrieved from Centers for Medicare & Medicaid Services: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html
- Centers for Medicare & Medicaid Services (CMS.gov). (2018). Quality Payment Program. Retrieved from Centers for Medicare & Medicaid Services: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-Quality-Payment-Program-webinar-slides-10-26-16.pdf